Lateral hip pain in Runners: Gluteal Tendinopathy overview
Gluteal tendinopathy, a condition affecting the tendons of the gluteal muscles around the hip, is a common source of lateral hip pain, among active and none active individuals. In this Blog we are going to focus on gluteal tendinopathy in runners. This condition can significantly impact daily activities, sleep, performance it is not easy to manage and is often misdiagnosed leading to sub optimal treatment, prolonging recovery. In this blog, we’ll explore what gluteal tendinopathy is, why it happens, and the most effective ways to manage and recover from it for runners.
What Is Gluteal Tendinopathy?
Gluteal tendinopathy refers to irritation or degeneration of the tendons that attach the gluteal muscles to the greater trochanter of the femur (the bony prominence on the side of your hip). The gluteus medius and gluteus minimus are the primary muscles involved, playing a crucial role in stabilising the pelvis and producing force during walking, running, squatting and other similar activities. When the tendons become overloaded or irritated through compressive or tensile loading, they can become painful, weaker and reduce your ability to perform sports or even daily tasks.
Common Symptoms
The hallmark symptom of gluteal tendinopathy is pain on the outer side of the hip, this can somemtimes coexist with ‘psudoradicular symptoms’ which is pain radiating down the outer thigh (this is one of the reasons it is often mistaken for Sciatica by both the general public and other healthcare professionals). Other common symptoms include:
An dull ache/ tight feeling on the lateral hip
Pain when lying on the affected side, often disturbing sleep.
Pain on prolonged deep sitting
Discomfort during prolonged standing (especially single leg), walking/running, or climbing stairs.
Tenderness to touch over the greater trochanter.
Increased pain with activities that involve higher gluteal loading, such as running or squatting.
Hangover symptoms - Often increase discomfort getting out of a chair/ walking a few hours after loading the hip.
Warm up effect - These symptoms tend to actually ease with a little bit of glute loading such as the start of the run, often leading to a false sense of tolerance and worsening of symptoms.
(Image: https://www.running-physio.com)
Why Does It Happen?
Gluteal tendinopathy typically results from one of/a combination of excessive or repetitive loading of the gluteal tendons, which doesn’t match the rate at which the body can recover from, anatomical and systemic health factors. Mechanical contributing factors include to this may include:
Overuse or Sudden Load Increase:
A increase in running, volume, frequency or intensity (speed/ hills) can overwhelm the tendons’ capacity to adapt.
Recovery:
Sleep, nutrition and hydration are the key foundations of recovery. These factors may play a vital role in how your body adapts to stressors and should be a key consideration when assessing overuse injuries. If these are not taken into account then it can lead to too much focus on little biomechanical loading
Previous Injury:
Especially to the same side can lead to compensations and abnormal loading during running.
Hormonal Factors:
Predominately in Women, especially post-menopausal women, may be more susceptible due to hormonal changes affecting tendon health, recovery and adaption.
(Image: https://e3rehab.com)
Sub optimal Hip and Pelvic Control during running:
Weakness in the gluteal muscles can lead to biomechanical changes during running such as a :
-contralateral pelvic drop during the stance phase
- excessive hip adduction during the swing phase.
Note: this does not mean that these running mechanics on their own cause symptoms
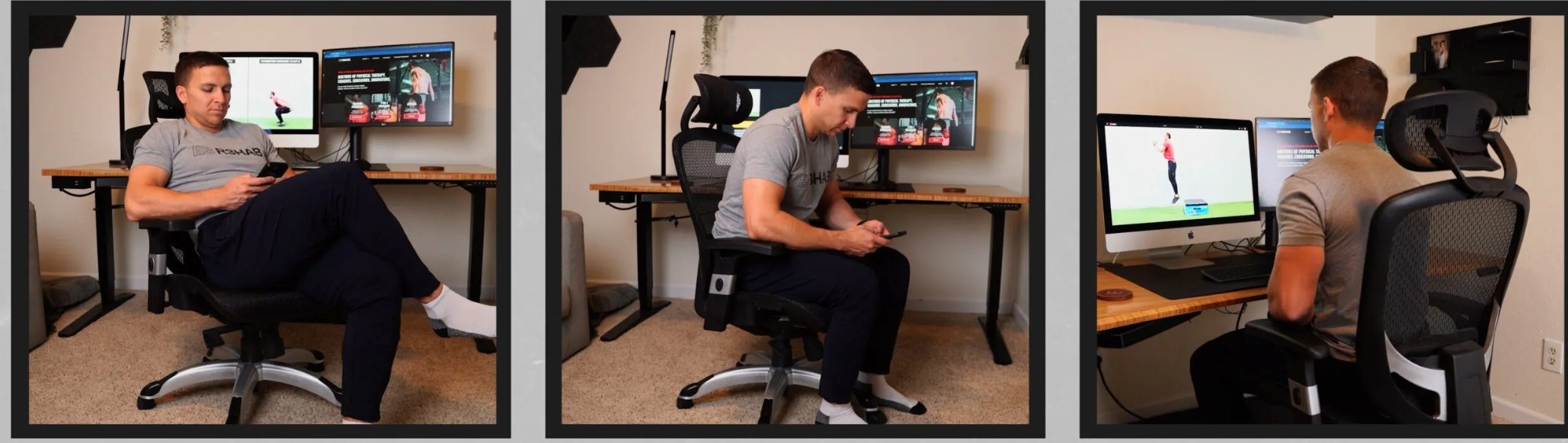
Compression:
Prolonged positions, such as sitting in a low chair, sitting cross-legged or standing with one hip popped out, can compress the tendons against the greater trochanter, exacerbating irritation.
(Image: https://e3rehab.com)
Diagnosis and Misconceptions
Diagnosing gluteal tendinopathy involves a thorough clinical assessment, often ruling out other potential causes of hip pain such as articular joint pathologies, BSI (Bone stress injuries) and referred lumbar pain. A common misconception is that gluteal tendinopathy is primarily due to inflammation. While inflammation may play a role, the condition is a lot more complex with that often with degenerative tendon changes and sensitisation of tissue. This means the focus of treatment should be on improving the health and function of the tendon rather than solely addressing inflammation through rest and NSAID’S.
Management and Recovery
The good news is that gluteal tendinopathy is treatable with a structured and patient-centered approach. Here are some key elements of effective management:
1. Assess current load and compressive capacity - (24hr pattern)
Initially, it’s essential to get an idea of how much load both compressive and tensile the tendons can tolerate. This is often done by reviewing how the symptoms react to these different types of loading and especially monitoring the 24hr response (due to the warm up and hangover effect previously mentioned). We can then make modifications to reduce any of these if needed. However, complete rest is not recommended as tendons need gradual loading to recover.
2. Focus on Optimal Loading
The cornerstone of treatment is a progressive loading program to strengthen the gluteal muscles and improve tendon capacity. This involves starting with low-load exercises that do not provoke pain and gradually progressing to higher-load, functional activities. Examples of early-stage exercises include:
Isometric gluteal contractions (e.g., holding a bridge position).
Side-lying leg lifts with controlled movement.
Monster walks
Single leg barbell hip thrust
As symptoms improve, exercises like squats, step-ups, and single-leg movements can be introduced.
(Image: https://e3rehab.com)
3. Address running mechanics (if necessary)
Altering running technique, especially foot strike pattern, cadence and hip adduction during the swing phase can lead to significantly less load on the gluteal tendon for the same amount of running. movement patterns, posture, and pelvic control can reduce unnecessary strain on the tendons. A physiotherapist can help identify and correct specific issues, such as excessive hip adduction or internal rotation during activities. However - remember that by offloading the lateral hip we are likely transferring that load elsewhere.
4. Manage Tendon Compression
Avoid positions and activities that compress the tendon, such as crossing your legs or sitting with your knees together to tolerable levels. Using cushions or pillows to support your hips when lying on your unaffected side can also help alleviate night-time pain.
5. Gradual Return to Activity
Reintegrating higher-impact activities, like running, should be done gradually and under professional guidance. Monitoring symptoms and adjusting training loads is essential to prevent flare-ups.
The Road to Recovery
Recovery from gluteal tendinopathy takes time and patience, with improvements often occurring over several months. Consistency with a tailored rehabilitation program and addressing contributing factors will maximize the chances of a full recovery. Working with a physiotherapist experienced in managing tendon conditions can provide the guidance and support needed to return to your favourite activities pain-free.
Final Thoughts
While gluteal tendinopathy can be a frustrating condition, understanding its causes and following an evidence-based approach to treatment can lead to significant improvements. By understanding your current capacity for load and matching that in daily life and sport you can often continue to do the things you love while rehabilitating the injured area. Patience, constancy, planning and progressive loading is absolutely key to successfully returning to 100% however, this must be individualised to your current symptoms, activity, goals, and contributing factors for the injury.